by Ian Birrell, Unherd:
Two years ago, over the Thanksgiving holiday, Allison Ducluzeau started to feel pain in her stomach. At first, she assumed she had eaten too much turkey, but the pain persisted. A couple of weeks later, she saw her family doctor who requested CT scans, although none were sorted. Soon after, as the agony worsened, her partner insisted she went to the emergency unit at their local hospital on Vancouver Island. Finally, doctors confirmed the couple’s worst fears: she was almost certainly suffering from advanced abdominal cancer.
TRUTH LIVES on at https://sgtreport.tv/
Allison, then 56, later learned that she had stage 4 peritoneal carcinomatosis, an aggressive condition. By the time she saw a specialist early last year, he warned that she might only live a few months longer: chemotherapy tended to be ineffective for her cancer, buying a bit more time at best, and she was inoperable. Instead, she was told to go home, sort out her papers, and decide if she wanted medical assistance in dying.
Unsurprisingly, Allison was devastated. “I could barely breathe — I went in there hoping to come out with a treatment plan but was just told to get my will in order.” That night was the worst of her life as she broke the shattering news to her son and daughter at her home in Victoria. “I told them I might only live for another two months,” she recalled. “If I’d not had my children, I might have accepted MAID [medical assistance in dying] — but when I saw the effect on them, having just been through the deaths of my own parents, it made me dig really deep.”
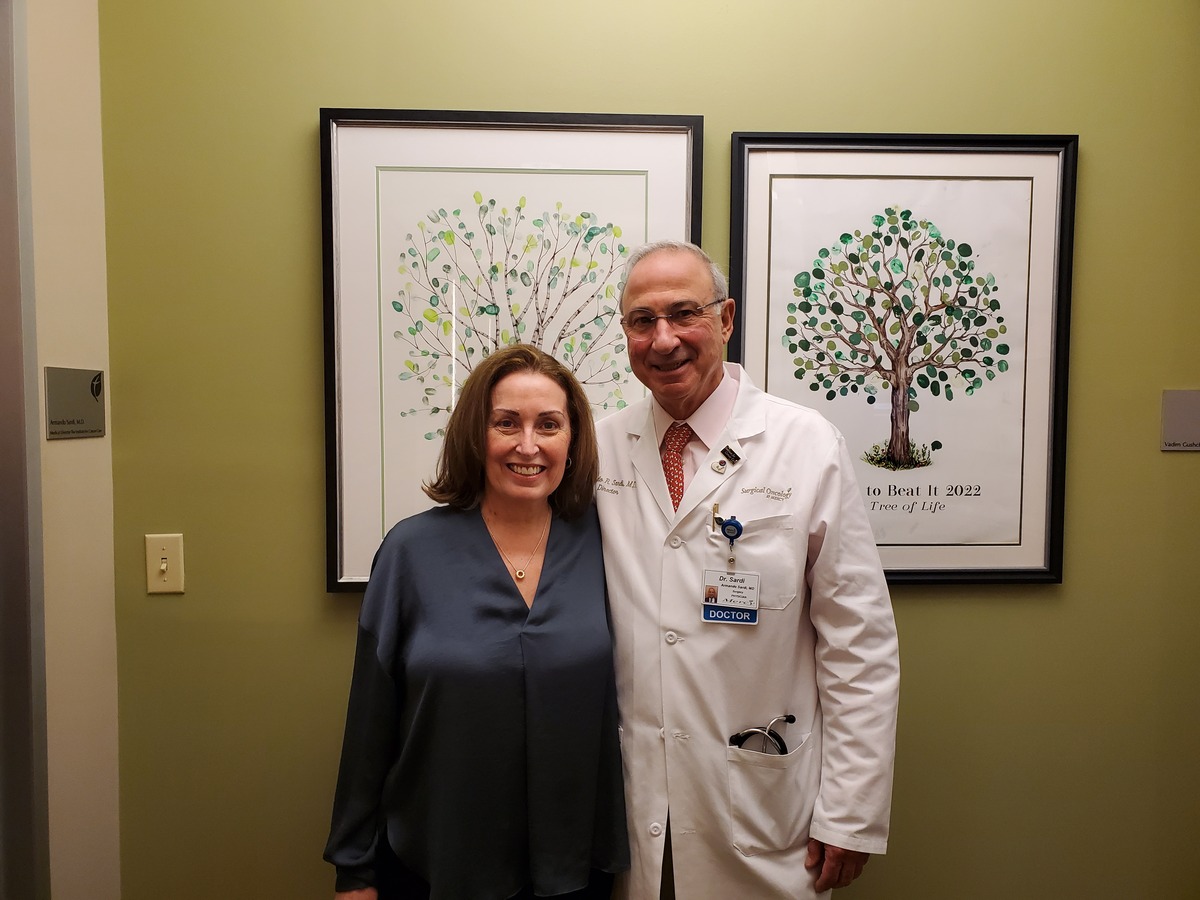
So, determined to find help, she researched her condition, spoke to doctors as far away as Taiwan, flew to California for scans and eventually travelled to Baltimore for treatment. She had discovered that patients could be given debulking surgery to reduce their cancer, followed by targeted use of heated chemotherapy — yet back in Canada, she could not get even an initial telephone chat with a surgeon who performed such operations for two months. Aided by her tight circle of friends and relatives, she raised almost half the $200,000 cost for the operation by crowdfunding. By the time she managed to see an oncologist in her home province of British Columbia, she was already on the road to recovery.
Today, Allison is in remission. She lifts weights daily, and goes running and cycling. She recently married her partner on a beach in Hawaii in front of her children. But she remains infuriated that Canadian doctors offered to kill rather than treat her. “The way it was presented was shocking,” she told me. “I was disgusted to be offered MAID twice. Once I was even on the phone, when I was on my own having just come back from Baltimore. It left me sobbing.”
As the debate over assisted dying heats up in Britain, with Keir Starmer promising a free vote on the matter if he wins the general election, and with politicians in Jersey approving plans for its use only last week, we should take notice of Allison’s case. For she does not share the ethical or religious concerns held by many opponents of euthanasia. Nor does she oppose Canada’s 2016 MAID reform; she agreed with her father five years later that it was an “appropriate” option for his intensifying pain after many years of prostate cancer.
But she has deep worries about assisted dying being offered by doctors in a health system that is floundering — especially with inadequate and overwhelmed oncology services when cancer patients comprise almost two-thirds of the soaring numbers of citizens opting for MAID. “We do not have a good standard of care here, especially for cancer — and that is why it is so dangerous to have MAID, especially when it can be used to take a bit of pressure off physicians and the government.” She knows of three other cancer patients whose families fear they died needlessly — including the person whose home she bought after downsizing to pay her medical bills in the US.
Allison’s very existence challenges those who argue that Britain — with its flailing health and social care systems, shamefully long waiting lists and historically poor cancer survival rates — should rush headlong into legalisation of assisted death. So, what would she tell those advocating for the reform? “I would tell Britain to only accept assisted dying when the health service is fixed — otherwise it is a very dangerous step to take. We deserve decent and timely care rather than offers of faster death.”



