by Brian Shilhavy, Health Impact News:
America has a huge drug addiction problem, where drug dealers are literally destroying this country.
No, I am not referring to fentanyl, meth, crack, heroin, or any other “illegal street drug” and the people who push them.
I am referring to the much larger drug addiction problem with drugs that are distributed by a much larger drug dealer network: FDA-approved and authorized prescription drugs.
TRUTH LIVES on at https://sgtreport.tv/
This is, by far, the largest criminal organization in the world. The pharmaceutical drugs distributed by medical doctors and purchased in drug stores that are on the corner of every city and town in America, are what is destroying this country.
These drugs are the leading cause of death in the United States, and their drug dealers are the largest class of criminal organizations in the world. See:
Pharmaceutical Industry is the Leading Cause of Death in U.S., and the Largest Criminal Group in the World
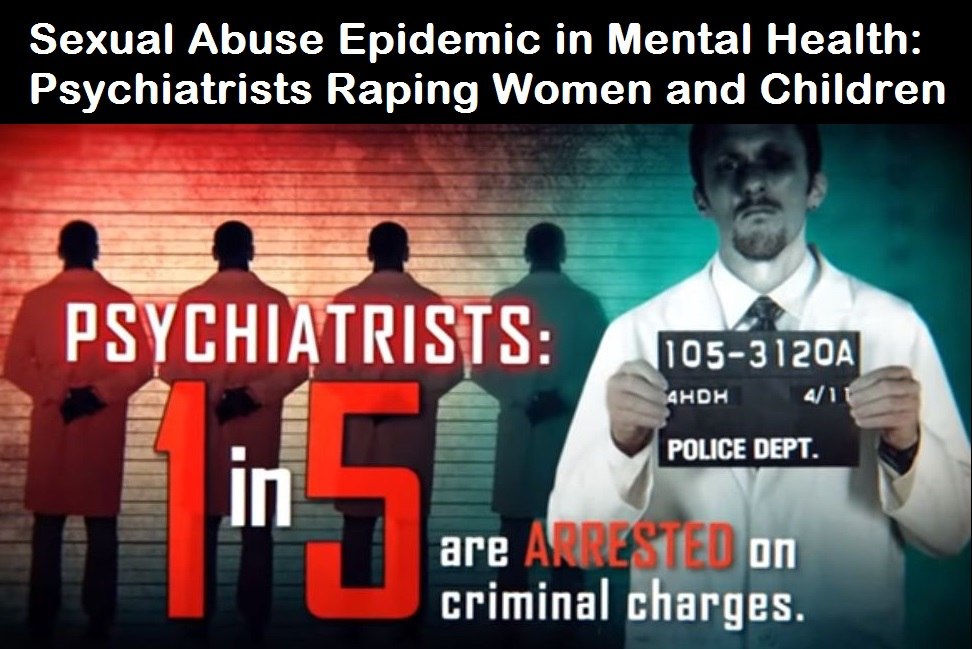
The worst offenders among these drug pushers, are the fake doctors called “psychiatrists,” where 1 out every 5 of these “doctors” are arrested on criminal charges, where 40% of all women in psychiatric wards are raped, and where a child is 3 times more likely to be sexually molested by a psychiatrist than by a stranger or registered sex offender.
For references to sources that back up these statistics, please see:
Sexual Abuse Epidemic in Mental Health: Psychiatrists Raping Women and Molesting Children
The holy grail of psychiatry that is used to justify pushing psych drugs onto people diagnosed with “mental illness,” including toddlers that are 2-3 years old, the “brain imbalance” theory, has been thoroughly debunked now by a study published last year in the journal Molecular Psychiatry:
The serotonin theory of depression: a systematic umbrella review of the evidence
This study caused a lot of outrage in the field of psychiatry, which is understandable as it rendered most psych drugs as useless and dangerous, and the study totally discredited the entire field of psychiatry as a fraud.
The authors waited almost a full year for all the criticisms to be sent in to them, and have now published their response:
The serotonin hypothesis of depression: both long discarded and still supported?
This study was not the first one to completely debunk the alleged “science” behind psychiatry.
Dr. Irving Kirsch, the associate director of the Placebo Studies Program at Harvard Medical School, published a book in 2011, titled: The Emperor’s New Drugs – Exploding the Antidepressant Myth.
Like most people, I used to think that antidepressants worked.
As a clinical psychologist, I referred depressed psychotherapy clients to psychiatric colleagues for the prescription of medication, believing that it might help.
Sometimes the antidepressant seemed to work; sometimes it did not.
When it did work, I assumed it was the active ingredient in the antidepressant that was helping my clients cope with their psychological condition.
According to drug companies, more than 80 per cent of depressed patients can be treated successfully by antidepressants.
Claims like this made these medications one of the most widely prescribed class of prescription drugs in the world, with global sales that make it a $19-billion-a-year industry.
Newspaper and magazine articles heralded antidepressants as miracle drugs that had changed the lives of millions of people.
Depression, we were told, is an illness – a disease of the brain that can be cured by medication.
I was not so sure that depression was really an illness, but I did believe that the drugs worked and that they could be a helpful adjunct to psychotherapy for very severely depressed clients. That is why I referred these clients to psychiatrists who could prescribe antidepressants that the clients could take while continuing in psychotherapy to work on the psychological issues that had made them depressed.
But was it really the drug they were taking that made my clients feel better?
Perhaps I should have suspected that the improvement they reported might not have been a drug effect. People obtain considerable benefits from many medications, but they also can experience symptom improvement just by knowing they are being treated.
This is called the placebo effect.
As a researcher at the University of Connecticut, I had been studying placebo effects for many years. I was well aware of the power of belief to alleviate depression, and I understood that this was an important part of any treatment, be it psychological or pharmacological.
But I also believed that antidepressant drugs added something substantial over and beyond the placebo effect. As I wrote in my first book, ‘comparisons of anti-depressive medication with placebo pills indicate that the former has a greater effect . . . the existing data suggest a pharmacologically specific effect of imipramine on depression’.
As a researcher, I trusted the data as it had been presented in the published literature. I believed that antidepressants like imipramine were highly effective drugs, and I referred to this as ‘the established superiority of imipramine over placebo treatment’.
The drug companies claimed – and still maintain – that the effectiveness of antidepressants has been proven in published clinical trials showing that the drugs are substantially better than placebos (dummy pills with no active ingredients at all).
But the data that Sapirstein and I examined told a very different story.
Although many depressed patients improve when given medication, so do many who are given a placebo, and the difference between the drug response and the placebo response is not all that great.
What the published studies really indicate is that most of the improvement shown by depressed people when they take antidepressants is due to the placebo effect.
Our finding that most of the effects of antidepressants could be explained as a placebo effect was only the first of a number of surprises that changed my views about antidepressants.
Following up on this research, I learned that the published clinical trials we had analysed were not the only studies assessing the effectiveness of antidepressants.
I discovered that approximately 40 per cent of the clinical trials conducted had been withheld from publication by the drug companies that had sponsored them.
By and large, these were studies that had failed to show a significant benefit from taking the actual drug. When we analysed all of the data – those that had been published and those that had been suppressed – my colleagues and I were led to the inescapable conclusion that antidepressants are little more than active placebos, drugs with very little specific therapeutic benefit, but with serious side effects. I describe these analyses – and the reaction to them – in Chapters 3 and 4.
I remain convinced that antidepressant drugs are not effective treatments and that the idea of depression as a chemical imbalance in the brain is a myth.
When I began to write this book, my claim was more modest. I believed that the clinical effectiveness of antidepressants had not been proven for most of the millions of patients to whom they are prescribed, but I also acknowledged that they might be beneficial to at least a subset of depressed patients.
During the process of putting all of the data together, those that I had analysed over the years and newer data that have just recently seen the light of day, I realized that the situation was even worse than I thought.
The belief that antidepressants can cure depression chemically is simply wrong. (Source.)
60 Minutes interviewed Dr. Irving Kirsch about his research. It’s less than 14 minutes long. This is on our Bitchute channel.
I know from the experience of covering this topic for over a decade now, that many of you reading this will be tempted to comment or email me and state something like this:
But Brian, you have no idea what it is like to live with depression and a mental illness, and these drugs have literally saved my life.
Wrong. I have battled depression my entire life, and I am a suicide survivor. I am now in my 60s, and I have never taken a single antidepressant pharmaceutical drug.
Read More @ HealthImpactNews.com



