by Will Jones, Daily Sceptic:

How might Covid vaccines reduce mortality?
There are two possible mechanisms, thoughtfully explained in a thorough review and a recent article on Brownstone: Covid vaccines might reduce the risk of infection, or reduce the risk of death — if infected, or both. We can explain the mechanisms in words, with reference to ‘marginal and conditional probabilities’, or we can depict them in a causal diagram — a powerful methodological tool.
TRUTH LIVES on at https://sgtreport.tv/
The first mechanism is simple: If a Covid vaccine reduces the risk of infection, it will also reduce the risk of death, because there is no doubt that getting infected increases the risk of death. Theoretical exceptions aside, if A affects B, and B affects C, then A affects C.
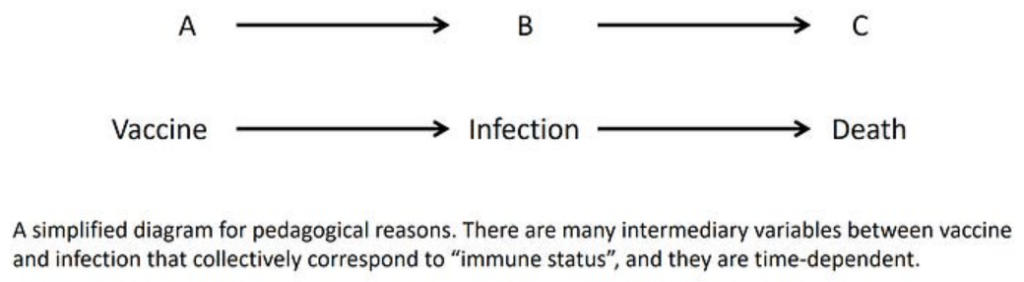
What if A does not affect B? What if a Covid vaccine does not reduce the risk of infection? Then it cannot reduce the risk of death through this mechanism. The causal chain does not exist. A link is broken.
By now we know that Covid vaccines appear temporarily to increase the risk of infection, and any subsequent benefit is nullified within months, if not turned again into harm (negative vaccine effectiveness). Therefore, according to the first mechanism, there is a short period when a Covid vaccine increases the risk of death, a limited period (a few months) when it decreases the risk of death, and a later period when the effect is null at best.
The second mechanism is more complicated. One aspect was explained in the Brownstone article and is related to a causal concept called ‘effect modification’. Like numerous epidemiological concepts, there are layers of complexity below superficial simplicity. I will keep it simple.
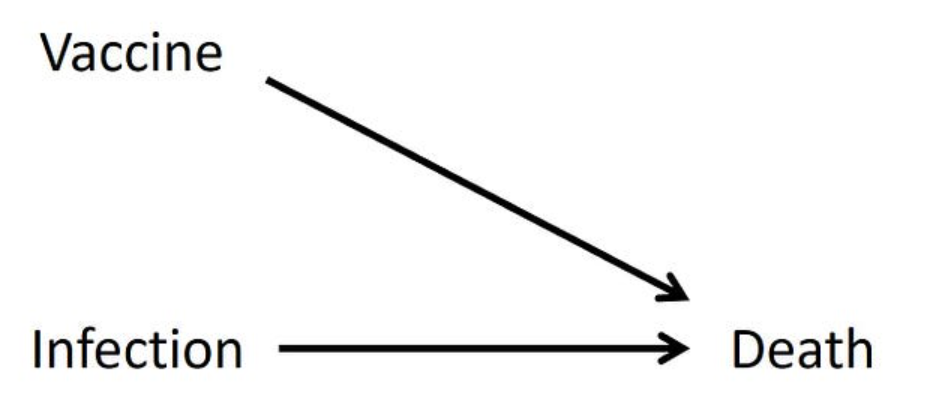
When two causes — Covid vaccine and Covid infection — operate on a single outcome (death), we may ask two causal questions:
- What is the effect of a Covid vaccine on the risk of death — if infected?
- What is the effect of a Covid vaccine on the risk of death — if not infected?
The second question is asking about vaccine-related death, the worst adverse effect. (A vaccine can be a cause of death even when someone is infected, but that’s another issue.)
Theoretically, the two types of effect could be different, in any possible way: magnitude and direction. Both might be harmful effects, yet of different magnitude. One might be beneficial and the other null, and so on. Add to that complexity time-varying effects, as noted earlier, and you can see how complicated causal reality might be.
Coincidentally, I encountered a relevant study at about the same time that I read the Brownstone article. That study provides insight into the two mechanisms by which Covid vaccines might reduce the risk of death, although the authors missed one aspect of their data (regarding reduced infections) and stopped short of the computation for the other (reduced mortality, if infected).
That’s not surprising. At times of biased media and biased science, we sometimes find insight from narrative-matched publications that missed interesting inference from the data.
Published as a ‘research letter‘, the study compared Covid mortality with mortality from seasonal flu. Using databases of the U.S. Department of Veterans Affairs (VA), the researchers identified patients who were hospitalised with an admission diagnosis of Covid or influenza and ascertained deaths. Most patients were elderly, the age group where Covid mortality is concentrated and effective vaccines are needed.
Did Covid vaccines reduce infections? Although the design was a classical retrospective cohort, the baseline data in the first table may be viewed as data from a hospital-based case-control study. (I cannot get into a technical explanation of ‘propensity score weighting’, but it can be ignored for a basic case-control analysis.)
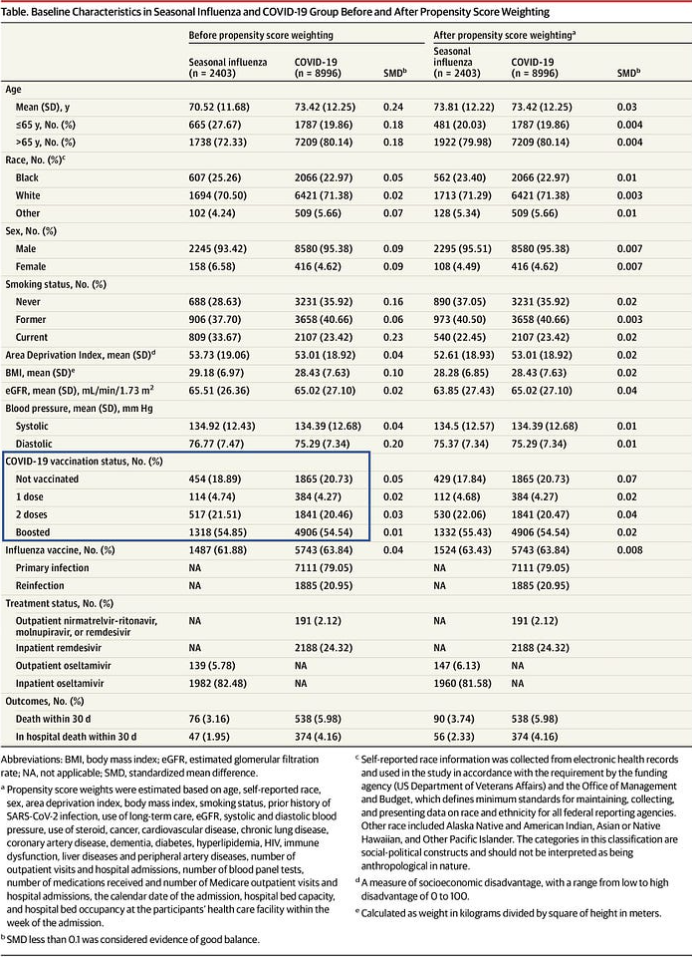
We may consider Covid patients as cases (numbering 8,996) and seasonal influenza patients as controls (there are 2,403). In a typical hospital-based case-control study, controls are selected from multiple disease categories, but I don’t see a major problem with this control group, and perhaps there are referral-related advantages.
Many complicated issues arise from a case-control study. Nonetheless, the basic analysis is simple. We visually compare the distribution of the suspected causal variable (Covid vaccination status) in cases and controls and compute odds ratios. If the vaccines meaningfully reduced the risk of infection, we should get odds ratios much smaller than 1.
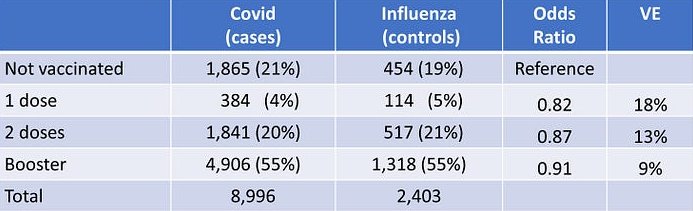
We have no such evidence in these data. The odds ratios are close to 1 (close to zero vaccine effectiveness) and they line up in the ‘wrong’ (unexpected) order of magnitude: the larger the number of doses, the weaker the apparent effect. The causal chain from vaccination to reduced mortality through reduced Covid infections is not corroborated.
Interestingly, we may also view influenza patients as cases and Covid patients as controls and compare the distribution of flu vaccination status in the two groups. Check their table above. There is no meaningful association either.



