by Anonymous Doctor, Daily Sceptic:

There follows a guest post by an NHS Emergency Department doctor on what, from his frontline vantage point, is behind the current hospital blockages and ambulance delays. This article first appeared on the website of the Health Advisory and Recovery Team (HART), a group of experts offering a second opinion on COVID-19 policy. Sign up for updates here.
As Emergency Department doctors, we were always going to be on the frontline. In spring 2020, we were taken to one side and it was suggested we might have to say goodbye to our relatives for the foreseeable future. Few realise the fear generated in hospitals in 2020. As Emergency Department consultants we were put on 24/7 emergency shift rotas and provided with vacant hotel rooms to live away from our families for their protection. Many of our colleagues left us to it and, soon after, patients arrived showing us signs that had been put up on their GP’s door saying “closed due to the pandemic”.
TRUTH LIVES on at https://sgtreport.tv/
Spring 2020 saw a combination of assessing and treating sick patients who had unusual and characteristic presentations of Covid in an otherwise quiet Emergency Department. The less-sick patients queued in their cars for assessment in the rapidly delivered ‘Covid-pod’. Huge hospital Covid signage was hastily erected. Doctors were redeployed to work in the Emergency Department from other specialties that were literally cancelled or scaled back hugely. I had one come to me at midnight asking why there were twice as many doctors in the place as patients; that he was bored and hadn’t seen a patient for three hours. Pre-lockdowns we were seeing over 300 patients each day. During the lockdown madness this dropped to less than 100 on some days. Many patients were petrified at the idea of coming to hospital. Others were instructed to stay away from the hospital unless extremely ill. This went on for months. Then the patients gradually came back, some with essentially no other access to healthcare. The department has not been quiet for some time now.
For many years now, my department (as with others throughout the U.K.) has been used as an overflow ward when beds cannot be found in the main hospital. Currently this is happening to an extent I have never previously experienced. A shortage of beds has been an issue for at least two of the three decades I have practised emergency medicine. It gets worse every year. The causes are multifactorial, but can be related to reduced numbers of beds or staff, decreasing access to community care, increasing waits for specialist referral and an elderly population whose primary (sometimes only) source of medical care is an emergency department. There is a major problem at the community discharge interface with patients waiting on packages of care, step-down wards, community beds and nursing homes. This exacerbates the bed cuts over the years and the centralisation of specialist services. I have heard of a hospital where one man will likely see his third Christmas as an inpatient. Patients are staying longer, and a lot are dying in hospital. These problems have just been exacerbated by ‘Covid Rules’, segregating the ‘Covid exposed’ from the ‘Covid recovered’ from the ‘Covid test positive’ from the ‘Covid test negative’ patients.
Emergency Department clinicians battle this with increasing frustration as the result is people essentially living in the department. Our department is back to seeing over 300 new patients per day and on one day last week we had over seventy patients living here awaiting hospital bed placement. Deaths in the department are increasing because sick people are remaining in the department for increasing lengths of time. The hardest bit is those needing end of life palliative care that get it delivered in the mayhem of an emergency department. It is very distressing for patients, staff and relatives.
Emergency departments operate as an outpatient interface between hospital and community. In the U.K., about the turn of the century (2000), most acute hospitals changed their admission arrangements from a GP referring to a specialty bed to a ‘single portal of entry’ arrangement. It was shrouded in the ‘safe and effective’ argument, but was a disaster on many levels. GPs no longer decided on admission; they decided on sending to the Emergency Department to decide on admission. The emergency departments were pulverised with a ‘four hour target’ for admission (under Blair’s Reforming Emergency Care). The media blamed emergency departments for ‘failing’ to meet the four hour target when, in effect, they were looking after the patients needing beds as well as serving emergencies.
The proper work of an emergency department is that of unscheduled care – people sourcing help in an emergency. The greater volume of work now is ‘processing’ admissions for inpatient specialties that don’t have beds for them. The Emergency Department is then expected to look after them, providing ward-level care (and sometimes intensive care) in corridors and rooms until a bed is available or they have been discharged (or left for heaven) from their Emergency Department trolley. (We have beds with hospital specialist mattresses for pressure sores in our corridors because of the long stays.)
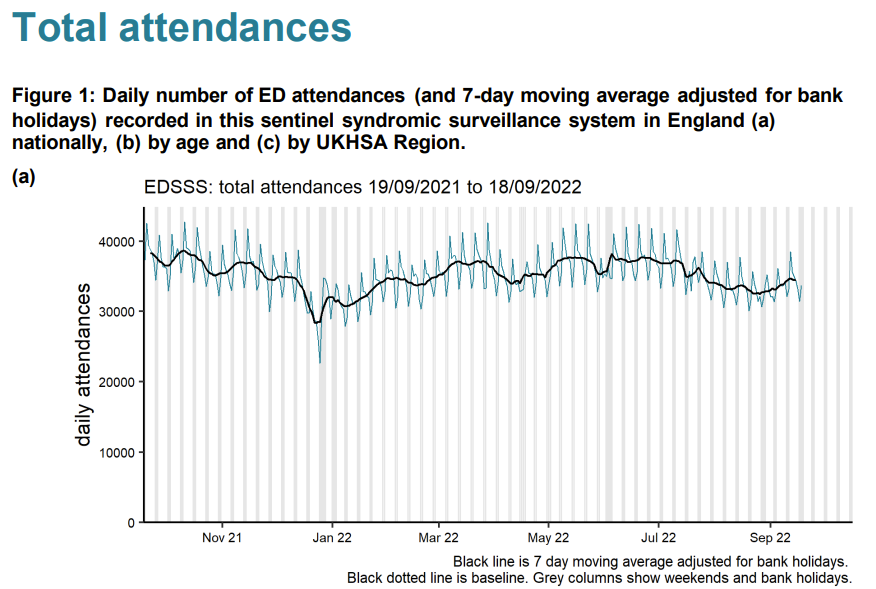
So, to say the numbers of admissions to emergency departments are lower than they were in the summer (as they currently are) gives no picture of the real congestion in emergency departments. You need to look at the number of patients waiting for beds. We are used to winter pressures with peaks and troughs. In 2021 we averaged 25 waiting in the department at a time (for at least a day) with no summer let-up. This year, for the same period, it is 45, with the worst summer ever. Emergency attendances are down – but admitted patients living in the department for days are more than doubled.
That aside, we have robust triage systems (stretched to the limit) where conditions that must be treated promptly are picked up within a target of 15 minutes of arrival (heart attacks, strokes, sepsis, haemorrhage etc.). The system is not perfect, but essentially these patients are identified as ‘time dependent conditions’ and brought to the Resuscitation Room for immediate assessment. Some are flagged by the Ambulance Service as ‘stand-by’ calls and sometimes paramedics take patients directly to where they can have, for example, urgent cardiology treatment to minimise damage from a heart attack. On the other hand, I am well aware of the recent problems with extensive delays in ambulance response times for some patients and occasions where the prioritisation has gone wrong.